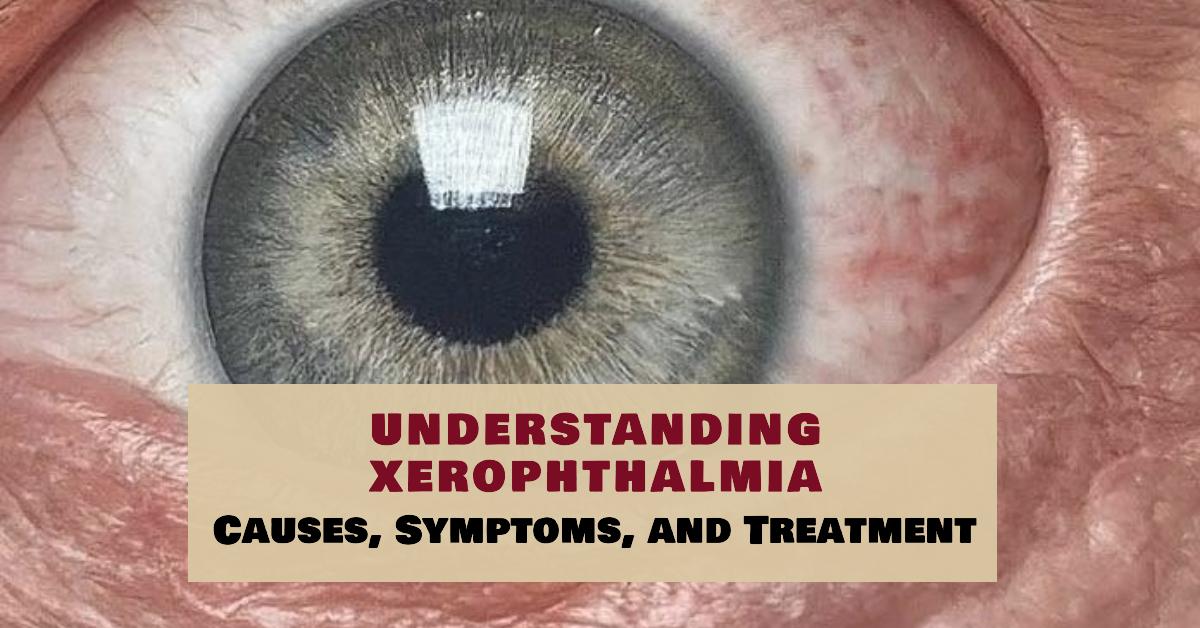
What is Xerophthalmia? Xerophthalmia is a medical condition characterized by extreme dryness of the eyes. It primarily results from a deficiency in vitamin A, which is crucial for maintaining the health and function of the eyes. When vitamin A levels are insufficient, the eye’s surface, including the cornea and conjunctiva, can become severely dry, leading to a range of symptoms and potential complications.
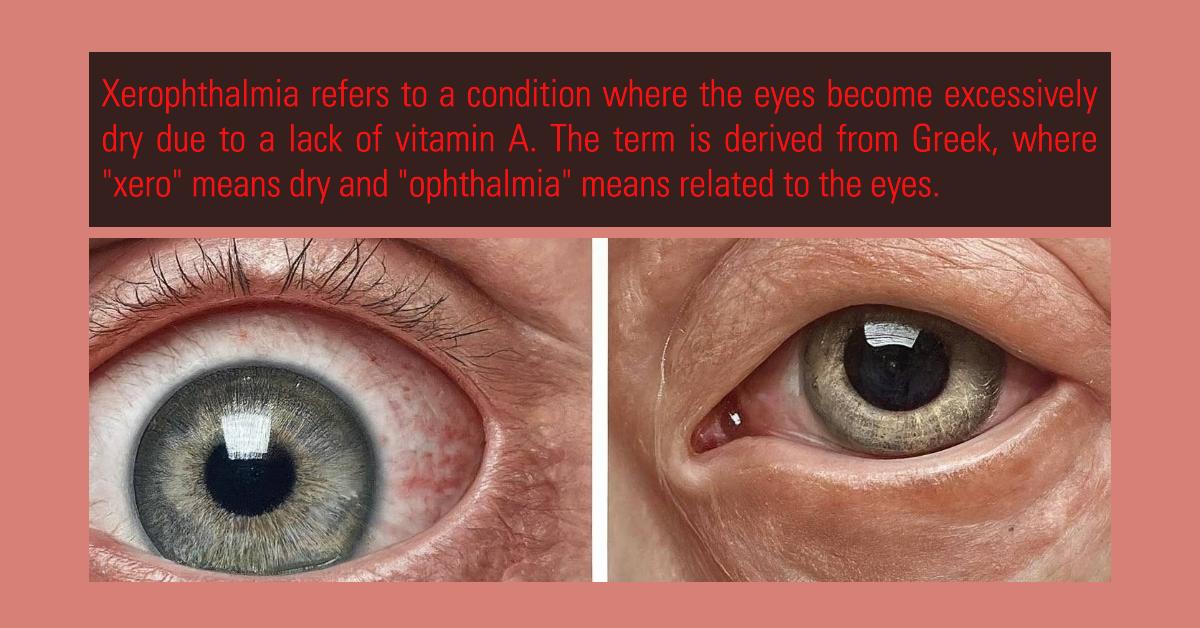
Definition – Xerophthalmia refers to a condition where the eyes become excessively dry due to a lack of vitamin A. The term is derived from Greek, where “xero” means dry and “ophthalmia” means related to the eyes.
Causes of Xerophthalmia
Xerophthalmia is primarily caused by a deficiency in vitamin A, which is essential for maintaining the health of the eyes and proper vision. Here’s a detailed look at the various causes of xerophthalmia:
1. Nutritional Deficiencies:
- Vitamin A Deficiency: The most common cause of xerophthalmia is a lack of vitamin A in the diet. Vitamin A is crucial for maintaining the health of the cornea and the production of tears. Diets low in vitamin A-rich foods—such as liver, eggs, dairy products, and colorful vegetables like carrots, sweet potatoes, and leafy greens—can lead to this deficiency.
2. Malabsorption Disorders:
- Celiac Disease: This autoimmune disorder damages the small intestine’s lining, affecting the absorption of nutrients, including vitamin A.
- Crohn’s Disease: An inflammatory bowel disease that can impair nutrient absorption, including vitamin A.
- Other Malabsorption Conditions: Conditions like cystic fibrosis and pancreatic insufficiency can also interfere with the absorption of vitamin A from the diet.
3. Chronic Diseases:
- Liver Disease: The liver plays a key role in processing and storing vitamin A. Chronic liver diseases, such as cirrhosis or hepatitis, can disrupt this process and lead to vitamin A deficiency.
- Kidney Disease: Severe kidney dysfunction can impact the body’s ability to maintain proper vitamin A levels.
4. Inadequate Diet:
- Poor Diet: In regions where diets lack variety or are heavily reliant on staple foods with low vitamin A content, deficiencies are more common. For instance, populations dependent on rice and other staples without sufficient fruits and vegetables are at risk.
5. Increased Vitamin A Requirements:
- Pregnancy and Lactation: Pregnant and breastfeeding women have higher vitamin A requirements. Without adequate intake, they can develop deficiencies that may lead to xerophthalmia.
- Growth Spurts: Children experiencing rapid growth may have increased vitamin A needs. Inadequate intake during these periods can lead to deficiencies.
6. Certain Medications and Treatments:
- Medications Affecting Vitamin A Absorption: Some medications or treatments can interfere with vitamin A metabolism or absorption, leading to deficiencies. For example, certain weight loss drugs that affect fat absorption might reduce vitamin A absorption.
7. Genetic Disorders:
- Genetic Conditions: Rare genetic disorders affecting vitamin A metabolism or transport, such as retinitis pigmentosa or certain inherited forms of night blindness, can contribute to xerophthalmia.
8. Environmental Factors:
- Exposure to Pollutants: Chronic exposure to environmental pollutants or harsh conditions can exacerbate dry eye symptoms and may contribute to the severity of xerophthalmia, especially in the context of an underlying vitamin A deficiency.
Understanding these causes can help in both the prevention and treatment of xerophthalmia by targeting the underlying issues leading to vitamin A deficiency. If you suspect a deficiency, consulting with a healthcare provider for proper diagnosis and treatment is essential.
Symptoms of Xerophthalmia
The symptoms of xerophthalmia can vary in severity and often progress if the underlying vitamin A deficiency is not addressed. Here’s a detailed overview of the symptoms associated with xerophthalmia:
Early Symptoms:
- Dryness: A persistent, uncomfortable feeling of dryness in the eyes is one of the first signs.
- Irritation: The eyes may feel gritty, scratchy, or irritated, as though there’s something in them.
- Redness: The eyes might appear red or inflamed due to dryness and irritation.
Progressive Symptoms:
- Night Blindness: Difficulty seeing in low light or darkness is an early sign of more severe vitamin A deficiency affecting vision.
- Xerosis: This refers to abnormal dryness of the conjunctiva, the thin membrane covering the white part of the eye and the inside of the eyelids.
- Corneal Damage: As the condition worsens, the cornea (the transparent front part of the eye) may begin to deteriorate. This can cause significant vision problems and discomfort.
- Bitot’s Spots: These are foamy, grayish patches on the conjunctiva, typically indicative of vitamin A deficiency.
- Keratomalacia: Softening of the cornea, which can lead to severe corneal damage and potential loss of vision.
- Corneal Ulcers: Open sores on the cornea that can be painful and affect vision.
Severe Symptoms:
- Permanent Vision Loss: Without treatment, the damage to the cornea can lead to irreversible vision loss.
- Secondary Infections: The compromised state of the cornea and conjunctiva can make the eyes more susceptible to infections.
If you or someone you know is experiencing these symptoms, it’s crucial to seek medical attention promptly to diagnose and address the underlying vitamin A deficiency and prevent further complications.
Diagnosing Xerophthalmia
Diagnosing xerophthalmia involves several steps to confirm the condition and identify its underlying cause. Here’s a detailed overview of the diagnostic process:
1. Medical History and Symptoms Review:
- Patient History: The healthcare provider will start by taking a thorough medical history. This includes asking about dietary habits, any symptoms of dry or irritated eyes, and any underlying health conditions that might affect vitamin A absorption or metabolism.
- Symptom Assessment: The provider will inquire about specific symptoms such as persistent dryness, irritation, redness, night blindness, and any recent changes in vision.
2. Physical Examination:
- Eye Examination: A comprehensive eye examination is performed to assess the condition of the eyes. This may include:
- Visual Acuity Tests: To measure how well the patient sees at various distances and identify any vision problems.
- Slit Lamp Examination: A special microscope (slit lamp) is used to examine the cornea, conjunctiva, and other structures of the eye. This helps in detecting dryness, Bitot’s spots, and corneal damage.
- Fluorescein Staining: Special dyes (such as fluorescein) are used to highlight any damage or dryness on the surface of the eye. The dye helps to reveal areas of corneal and conjunctival damage.
3. Laboratory Tests:
- Blood Tests: To measure serum vitamin A levels and assess if a deficiency is present. Blood tests help determine whether vitamin A deficiency is contributing to the symptoms.
- Other Tests: Depending on the suspected underlying causes, additional tests might be performed to evaluate for malabsorption disorders or chronic diseases that affect vitamin A metabolism.
4. Differential Diagnosis:
- Ruling Out Other Conditions: The healthcare provider will consider other potential causes of dry eyes or vision problems, such as:
- Dry Eye Syndrome: Often caused by factors other than vitamin A deficiency.
- Autoimmune Disorders: Conditions like Sjögren’s syndrome that affect tear production.
- Infections or Allergies: These can also cause eye dryness and irritation.
5. Specialized Tests (if needed):
- Imaging Studies: In some cases, imaging studies might be used to assess the extent of corneal damage or other eye structures.
- Tear Production Tests: Tests like the Schirmer test measure the amount of tears produced to differentiate between xerophthalmia and other dry eye conditions.
6. Diagnosis Confirmation:
- Confirming Xerophthalmia: If vitamin A deficiency and its associated symptoms are confirmed, the diagnosis of Xerophthalmia is established. The healthcare provider will then focus on treating the deficiency and managing the symptoms.
7. Follow-Up:
- Monitoring Progress: After initiating treatment, regular follow-up appointments are important to monitor the patient’s response to therapy, reassess vitamin A levels, and ensure that symptoms are improving.
Accurate diagnosis is crucial for effective treatment and management of xerophthalmia. Addressing both the vitamin A deficiency and any underlying causes will help alleviate symptoms and prevent potential complications.
Treatment and Prevention of Xerophthalmia
Treatment of Xerophthalmia:
- Addressing Vitamin A Deficiency:
- Dietary Changes:
- Increase Vitamin A Intake: Incorporate foods rich in vitamin A into the diet. Key sources include:
- Animal Sources: Liver, eggs, and dairy products.
- Plant Sources: Carrots, sweet potatoes, spinach, kale, and other colorful vegetables. These contain provitamin A carotenoids like beta-carotene, which the body can convert into vitamin A.
- Vitamin A Supplements:
- Oral Supplements: High-dose vitamin A supplements may be prescribed by a healthcare provider to rapidly correct deficiencies. The dosage will depend on the severity of the deficiency and the patient’s specific needs.
- Supplement Form: Vitamin A supplements are available in various forms, including capsules, tablets, and liquids. The form and dosage should be guided by a healthcare provider to avoid toxicity.
- Dietary Changes:
- Managing Eye Symptoms:
- Artificial Tears and Lubricants
- Eye Drops: Use over-the-counter artificial tears or lubricating eye drops to relieve dryness and irritation. These help to mimic natural tears and provide temporary relief.
- Ointments: In more severe cases, thicker lubricating ointments might be recommended, especially for overnight use.
- Avoid Irritants:
- Environmental Controls: Protect eyes from irritants like smoke, dust, and wind. Use sunglasses or protective eyewear as needed.
- Artificial Tears and Lubricants
- Treating Complications:
- Eye Infection Management: If xerophthalmia has led to eye infections or corneal ulcers, appropriate treatments, such as antibiotics or antiviral medications, may be required.
- Surgical Interventions: In severe cases with corneal damage or keratomalacia, surgical interventions might be necessary to repair the cornea or address complications.
Prevention of Xerophthalmia:
- Adequate Nutritional Intake:
- Balanced Diet: Ensure a diet rich in vitamin A and other essential nutrients. A variety of fruits, vegetables, and animal products should be included to maintain optimal vitamin A levels.
- Fortified Foods: In some regions, foods fortified with vitamin A can help address deficiencies, particularly in populations at risk.
- Monitoring and Management:
- Regular Health Check-Ups: Routine medical and eye examinations can help detect early signs of vitamin A deficiency and other health issues before they become severe.
- Addressing Malabsorption Issues: If you have conditions that affect nutrient absorption, work with healthcare providers to manage these disorders and ensure adequate vitamin A intake.
- Educational and Public Health Initiatives:
- Community Programs: Public health programs can educate communities about the importance of vitamin A and how to prevent deficiencies through diet and supplementation.
- Supplementation Programs: In areas where vitamin A deficiency is prevalent, government or NGO-led supplementation programs may be implemented to provide vitamin A to at-risk populations, such as children and pregnant women.
- Healthy Lifestyle:
- Hydration: Maintain good hydration to support overall eye health.
- Eye Protection: Use sunglasses to protect your eyes from UV rays and environmental irritants, which can exacerbate dryness.
By focusing on these treatment and prevention strategies, xerophthalmia can be effectively managed and prevented, ensuring better eye health and overall well-being. Regular check-ups and a balanced diet are key to maintaining adequate vitamin A levels and preventing the development of xerophthalmia.
Frequently Asked Questions about Xerophthalmia
- What are the early signs of xerophthalmia?
- Early signs include persistent dryness, irritation or gritty sensations, and redness. Consult a healthcare provider for a diagnosis if these symptoms occur.
- Can xerophthalmia lead to permanent vision loss?
- Yes, untreated xerophthalmia can cause corneal damage and permanent vision loss. Early diagnosis and treatment are essential to prevent severe complications.
- How is xerophthalmia treated?
- Treatment involves addressing vitamin A deficiency through dietary changes, supplements, and using lubricating eye drops for relief.
- Is xerophthalmia preventable?
- Yes, it can be prevented by maintaining a diet high in vitamin A and having regular eye check-ups.
- Are there any lifestyle changes that can help manage xerophthalmia?
- Staying hydrated, using protective eyewear, and maintaining a balanced diet with essential nutrients are effective for managing and preventing xerophthalmia.
Conclusion Xerophthalmia is manageable with proper care and early treatment. By understanding its causes, symptoms, and treatment options, you can take proactive steps to maintain your eye health and prevent complications.