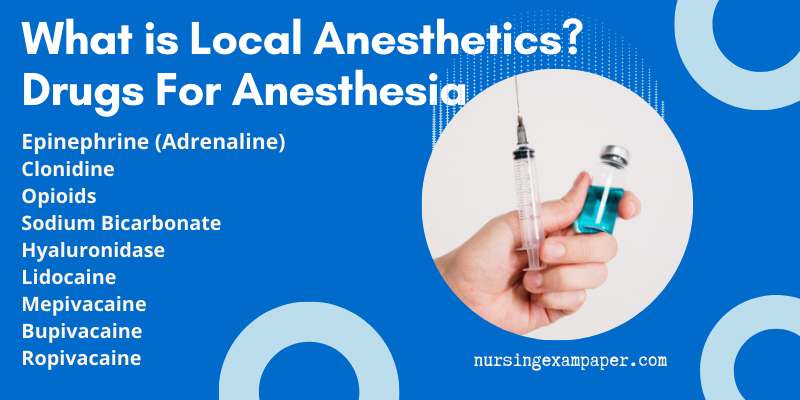
What is Local Anesthetics? – There are a number of local anesthetics available for use with regional anesthesia including lidocaine, mepivacaine, chloroprocaine, prilocaine, etidocaine, bupivacaine tetracaine, and ropivacaine. They each have their advantages and disadvantages as well as different times of onset and durations of action. We have limited our practice to the use of four local anesthetics, lidocaine and mepivacaine (short onset and duration of action) and bupivacaine and ropivacaine (longer onset and duration of action). With the exception of distal blocks, we often add epinephrine to the local anesthetic solutions (premixed solutions containing epinephrine are acidic) to increase the safety margin of each local anesthetic, therefore allowing for a higher recommended maximum dose.
What uses of Local Anesthectics?
The combination of two local anesthetics such as lidocaine or mepivacaine and bupivacaine or ropivacaine for the blockage of a nerve at multiple sites provides the benefits of both agents: a short onset of action and a duration of action of at least 10 to 12 hours, and often more. Thus, peripheral nerve blocks can be performed without much concern for operating room delays, and adequate postoperative analgesia can be provided without the need for continuous local anesthetic infusions. If longer postoperative analgesia is warranted, a catheter is placed, with the use of a nerve stimulator, before surgery and perfused with a solution of 0.125% bupivacaine or 0.2% ropivacaine at a rate of 10 to 15 ml/hr. Finally, if a short-duration block is required, 1% lidocaine or mepivacaine with epinephrine is indicated.
Lidocaine, mepivacaine, bupivacaine, and ropivacaine can produce central nervous system toxicity (i.e., seizure, loss of consciousness, tinnitus). All local anesthetics (bupivacaine > ropivacaine) can produce cardiac toxicity. Ropivacaine appears to be up to fourfold less toxic than bupivacaine. This lower toxicity is an important consideration for replacing bupivacaine with ropivacaine in our practice.
Arrhythmias produced by bupivacaine are often ventricular in nature and associated with fatal outcomes because they are rarely reversible. The toxicity of local anesthetics can be immediate or delayed (within 45 minutes after injection). Consequently, patients need to be monitored carefully for at least 1 hour after injection of local anesthetic solutions. To minimize the toxicity associated with overdosage related to complementary injections made to perfect the block, a waiting period of at least 10 to 20 minutes before a second injection is recommended.
Low Back Pain (LBP) – Type, Causes, Diagnosis & Management by Dr. Rahul Garg
How to use Local Anesthetics?
In most cases, we use a combination of 1.5% lidocaine or mepivacaine with epinephrine and 0.5% bupivacaine with epinephrine or 0.75% ropivacaine. We add 1 ml of molar sodium of bicarbonate for every 10 ml of lidocaine to shorten the onset of the block. For upper extremity blocks, this shortens the onset to 5 to 10 minutes. However, it usually takes 10 to 15 minutes for the block to become optimal. For lower extremely blocks, the onset time is longer and varies according to the nerve being blocked. It takes 10 to 15 minutes for a femoral block, and at least 20 to 30 minutes, possibly longer, for a sciatic block.
To minimize complications resulting from intravascular injection of a local anesthetic solution, aspiration should be performed and repeated after each 5 ml of local anesthetic solution injected.
Some New Drugs Added to Local Anesthetics
The main purpose of adding these new drugs to local anesthetics is as follows
- To reduce the latency of the block onset.
- To improve the quality of the block.
- For prolong the duration of analgesia.
- Reduce the doses of local anesthetics.
Revotaz Injection Properties, Uses, Adverse effect
1. Epinephrine (Adrenaline)
Site of Action – Local.
Mechanisms – Slowed blood absorption of the local anesthetic agent because epinephrine induces local vasoconstriction.
Main Effects of Epinephrine
Prolonged duration of the block. Duration may be increased from 30% to 50%, depending on the vasculature at the site of injection. The best effects are obtained with intrapleural anesthesia.
Other Effects of Epinephrine
Reduction of the inherent toxicity of local anesthetics. Peak plasma concentration may be reduced up to 50%.
Adverse Effects Epinephrine
Hemodynamic effects if massive blood absorption or intravascular injection. Tachycardia or arrhythmia indicates an inadvertent intravascular placement of the needle or catheter and necessitates the immediate cessation of local anesthetic injection.
Oseltamivir Phosphate Uses, dose, mechanism and effects
Dose – 5μg/ml (1/200,000).
How to use of Epinephrine
All peripheral blocks, except those in the vicinity of extremities because of terminal arterial blood flow. For example, epinephrine is contraindicated in penis block and usually in arthritic patients or those with scleroderma.
2. Clonidine Injection as a Local Anesthetics
Clonidine is the only α2-agonist used in combination with local anesthetics. Its use is well documented.
Site of Action – Local, but also central after blood absorption from the nerve sheath.
Mechanisms – Weak local anesthetic action of the α2-agonist itself, but possibility of synergistic interaction with local anesthetics.
Main Effects of Clonidine Injection
Prolonged duration of anesthesia and analgesia that follows neural blockade, depending on the potency of local anesthetics used. Anesthesia may be prolonged by 30% to 50% with mepivacaine supplemented with 150 μg clonidine. Analgesia may be prolonged by 40% to 400% depending on the clonidine dose.
Other Effects of Clonidine Injection
Added to lidocaine, clonidine can also reduce the onset time, extend the sensory block, and improve its quality at the time of surgery.
Asthma, types symptoms day and theme
Adverse Effects of Clonidine Injection
Sedation is the main and often the sole adverse effect. This must be taken into consideration in a premedicated patient. It is best to avoid premedication or to reduce it in a patient with anxiety over the block. Other effects include decreased blood pressure and slowed heart rate Rarely, there is_an abnormal ventilatory patters.
Dose – The minimum dosage, which results in significant prolongation of anesthesia, is 0.5 μg/kg. Increasing the dose of clonidine results in a greater number of adverse effects. The best compromise is a clonidine dose of 75 μg.
Use of Clonidine – All peripheral nerve blocks.
3. Opioids
There is cytochemical and behavioral evidence that opioids may have effects on peripheral nerves. Whether such an effect may improve clinical neural blockade and analgesia is debated. Inflammatory phenomena, history of chronic pain, and site of injection might account for controversy. Results are conflicting.
Site of Action – Local, but also central.
Mechanisms of Opioids – Hypothetical effect on axonal opioid receptors. Action on spinal cord either by diffusion or by centripetal axonal transport also has been invoked.
Main Effects – Analgesia lasting several hours, unrelated to the opioid dose injected.
Other Effects – Reduction in the time of block onset using derivatives with high lipid solubility.
Adverse Effects – Nausea and vomiting; some cases of pruritus.
Dose of Opioids – For example, 3 to 5 mg morphine could prolong analgesia up to 36 hours. A 50% reduction in the dose of postoperative analgesic may be obtained by adding 0.1 mg/’kg morphine to lidocaine.
Uses of Opioids – Documented only for brachial plexus blocks.
4. Sodium Bicarbonate
Site of Action – Local.
Mechanisms of Sodium Bicarbonate
Local anesthetics penetrate nerve cell membranes in their nonionized form and act intracellularly in the ionized form. Because local anesthetics are weak bases, addition of sodium bicarbonate increases their pH to the physiologic range, thus decreasing the ionized/nonionized ratio. This results in both an increased rate of penetration and a greater total mass of local anesthetic in the nerve. An anesthetic effect of bicarbonate itself has also been suggested.
Main Effects of Sodium Bicarbonate
There is a 30% to 50% reduction in onset time (i.e., approximately a 4-minute reduction with mepivacaine, 8 minutes with lidocaine, and 14 minutes with bupivacaine). The extent and quality of the block are improved.
Other Effects – Prolonged duration of analgesia has also been reported.
Adverse Effects – Unknown.
Dose of Sodium Bicarbonate – To adjust the pH of local anesthetic solutions to the physiologic range.
Uses of Sodium Bicarbonate – All peripheral nerve blocks.
5. Hyaluronidase
Site of Action – Local.
Mechanisms – Enzyme acting on hyaluronic acid, a component of several connective tissues. Hyaluronidase liquefies the interstitial barriers and increases the spread of local anesthetic solutions through tissue planes.
Effects – Reduction of onset time (not evaluated).
Adverse Effects – Rare cases of allergy.
Dose – Not clearly established, from 50 to 150 units.
Use – Ophthalmic procedures.
Thanks.
ESIC Exam Paper Staff Nurse Feb 2019
Reference – Peripheral Nerve Blocks – A Color Atlas Edited by Jacques E. Chelly,
Page no. 12-14.