Cesarean section is a surgical procedure in which a baby is born through an incision made in the abdomen and uterus. This procedure is also known as C-section/Caesarean delivery.
Cesarean section is done because vaginal delivery is not safe for mother and baby in many situations Such as breech birth, placenta previa, and high blood pressure.
The cesarean section usually takes 45 minutes to 1 hour. and is usually performed with spinal anesthesia and also with general anesthesia.
Here’s a detailed overview of the procedure, its types, indications, complications, and post-operative management:

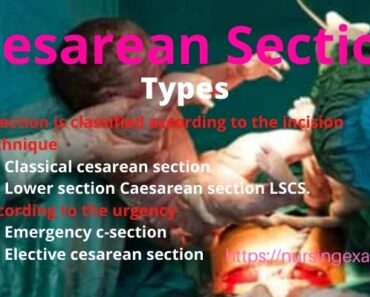
Types of Cesarean Section / C Section Surgery –
C section is classified according to the incision technique
- classical cesarean section
- Lower section Caesarean section LSCS.
According to the urgency
- emergency c-section
- elective cesarean section
Classical cesarean section
In a classical cesarean delivery, a vertical incision is made in the midline of the abdomen. Once the abdomen is incised, the uterus is also incised vertically and the baby is delivered.
The classical C Section is not commonly used now, because it requires a large amount of space for delivery. The classical incision increases the risk of hernia. because long incisions can weaken the abdominal muscles.
Causes of classical Cesarean Section or indication for Classical Cesarean
- Preterm labor
- Dense adhesion
- Placenta previa
- Placenta accreta
To decrease the risk of hemorrhage and adhesion
Preterm labor – In preterm labor lower uterine segment is not developed to provide adequate space for fetal delivery.
Fetal malformations like – macrocrania sacrococcygeal teratoma and conjoined twins.
Transverse lie and breach.
The procedure of classical cesarean
A midline vertical incision is chosen for laparotomy, classical incision provides a quick and short interval between incision and delivery.
There is less blood loss in this incision, which provides more space for the procedure.
The disadvantage of the classical section
- Poor/bed cosmetic results.
- Incisional hernia.
- More postoperative pain.
Lover Segmental Cesarean Section/bikini cut –
Introduction – this procedure is the most commonly used type of C section, a transverse incision is made in the lower uterine segment. for delivery of the baby. in this type of incision feeling of incision is more efficient than in others. And it has less blood loss.
Emergency C section
An emergency C-section is required in some conditions such as
- Previous cesarean delivery
- Placenta previa
- Placenta accrete
- Fetal distress
- Antepartum eclampsia
- Multiple fetuses
Elective C section
Some surgery is scheduled in advance, so it does not involve a medical emergency. some women do not want normal vaginal delivery of the baby.
Causes of cesarean section indication
- Delayed labor if the cervix is not open enough after several hours of a strong contraction. then Cesarean Section is necessary.
- Fetal distress baby heartbeats decrease then C Section is necessary.
- Abnormal positions – transverse lie, breach lie, shoulder presentation.
- Multiple fetuses- twins, triple, and more babies.
- Placenta previa
- placenta acreta
- Cord loop around baby’s neck and cord prolapse
- Women who have heart and brain problems
- Hydrocephalus
- Previous cesarean delivery.
Complications of cesarean section
- Infection in the lining of the uterus
- Postpartum hemorrhage
- Blood clots
- Surgical injuries urinary bladder Rapture and bowl rupture
- Wound infection
- Reaction of anesthesia
- DVT deep vein thrombosis
Nursing Management after the C-section
Nursing management after a cesarean section (C-section) is crucial for ensuring the patient’s recovery, managing complications, and facilitating a smooth transition to postpartum care. Here’s a comprehensive guide to nursing management following a C-section:
Immediate Postoperative Care
- Monitoring Vital Signs:
- Frequency: Check frequently in the immediate postoperative period, then less frequently as the patient stabilizes.
- Parameters: Monitor temperature, blood pressure, heart rate, and respiratory rate.
- Rationale: Early detection of complications such as infection, bleeding, or changes in cardiovascular status.
- Assessment of the Surgical Site:
- Inspection: Regularly inspect the incision site for signs of infection, dehiscence (opening of the wound), or hematoma.
- Dressing: Ensure the dressing is clean, dry, and intact.
- Rationale: Early identification of complications can help prevent serious issues and facilitate prompt treatment.
- Pain Management:
- Assessment: Regularly assess pain using a pain scale and evaluate the effectiveness of pain relief measures.
- Medications: Administer prescribed analgesics, which may include opioids, non-opioid analgesics, or local anesthetics.
- Non-Pharmacological: Encourage relaxation techniques, repositioning, and application of heat or cold if appropriate.
- Rationale: Effective pain management enhances comfort, promotes mobility, and supports recovery.
- Monitoring for Complications:
- Bleeding: Monitor lochia (postpartum vaginal discharge) for volume and characteristics, and check for signs of excessive bleeding from the incision site.
- Infection: Observe for signs of infection such as fever, increased redness, swelling, or discharge from the wound.
- Thrombosis: Watch for signs of deep vein thrombosis (DVT), such as swelling, redness, or pain in the legs.
- Rationale: Prompt recognition and intervention can prevent serious complications and ensure patient safety.
Postoperative Care
- Encouraging Mobility:
- Activity: Encourage the patient to begin moving as soon as it is safe, typically within 24 hours post-surgery.
- Support: Assist with early ambulation and provide support to minimize discomfort and prevent complications such as DVT and constipation.
- Rationale: Early mobilization promotes circulation, reduces the risk of complications, and aids in overall recovery.
- Hydration and Nutrition:
- Diet: Initially start with clear liquids and gradually advance to a regular diet as tolerated.
- Hydration: Ensure adequate fluid intake to prevent dehydration and support overall health.
- Rationale: Proper nutrition and hydration support healing and energy levels.
- Wound Care:
- Care: Educate the patient on how to care for the incision site, including how to keep it clean and dry.
- Follow-Up: Arrange for follow-up appointments to monitor wound healing and address any concerns.
- Rationale: Proper wound care reduces the risk of infection and promotes optimal healing.
- Breastfeeding Support:
- Assistance: Provide support and education on breastfeeding techniques, especially in managing positioning and comfort post-surgery.
- Support: Address any challenges related to breastfeeding and offer resources or referrals as needed.
- Rationale: Supporting breastfeeding helps with maternal-infant bonding and provides optimal nutrition for the newborn.
- Education and Emotional Support:
- Education: Educate the patient about signs of complications, pain management, care of the incision, and the importance of follow-up care.
- Emotional Support: Provide emotional support and reassurance, addressing any anxiety or concerns the patient may have about recovery or caring for the baby.
- Rationale: Comprehensive education and emotional support enhance patient confidence and promote a positive recovery experience.
- Monitoring Urine Output:
- Assessment: Regularly monitor urine output and ensure adequate hydration.
- Rationale: Adequate urine output indicates proper hydration and kidney function, and helps identify potential complications such as urinary tract infections.
Long-Term Considerations
- Discharge Planning:
- Instructions: Provide clear discharge instructions, including signs of complications, follow-up care, and activity restrictions.
- Support: Arrange for community resources or home health care if needed.
- Rationale: Effective discharge planning helps ensure a smooth transition from hospital to home and promotes continued recovery.
- Follow-Up Care:
- Appointments: Schedule and confirm follow-up appointments with the healthcare provider.
- Support: Encourage the patient to attend follow-up visits for ongoing assessment and care.
- Rationale: Regular follow-up helps monitor recovery progress and address any issues that may arise post-discharge.
By adhering to these guidelines, nurses can provide comprehensive care that supports the physical and emotional well-being of the patient after a cesarean section, facilitating a smooth recovery and promoting overall health.
Also Read –
Placenta Previa: Its Types and Management
The Pregnancy Period Third Trimester
Dengue fever Symptom Treatment and Prevention
What are the Placenta Types and Functions





Nursing model question paper with answer post basic BSc nursing entrance exam question paper PDF