Introduction of Postpartum hemorrhage (PPH)
Postpartum hemorrhage (PPH) is a critical medical condition characterized by significant blood loss through vaginal bleeding following childbirth. This condition poses a serious threat to maternal health and typically occurs immediately after the delivery of the placenta, though it can also manifest up to 12 days post-delivery. PPH requires prompt recognition and intervention due to its potential to rapidly escalate and cause severe complications. Understanding its causes, risk factors, symptoms, and effective management strategies is crucial for timely and effective clinical response to safeguard maternal well-being.
Types of PPH:
Primary PPH: Occurs within the first 24 hours after delivery.
Secondary or late PPH: Occurs 24 hours to 12 weeks postpartum

Cause of PPH
PPH causes are described in some points given below-
- Atonic uterus – The uterus contracts after delivery, and pushes the placenta out as a placental delivery. These contractions help put pressure on the blood vessels in the area of placental attachment. These contractions give a tone to the uterus. When the uterus does not contract strongly, bleeds freely through the blood vessels. This is called an atonic uterus.
- Cervical and vaginal tear.
- Tear in the uterine blood vessels.
- Blood clotting disorder.
- low platelets or increased INR.
- Placenta problems (abnormal placentation)
- The tissue of the placenta that stays attached to the uterus may cause PPH.
Risk factors for postpartum hemorrhage
Below points are the major risk factors for PPH –
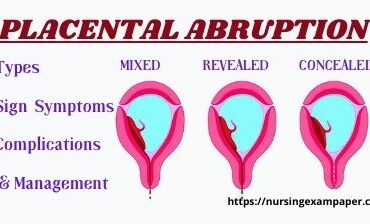
- Placental abruption.
- Placenta previa.
- Over distended uterus:- Large uterus due to big baby and polyhydramnios (more uterine fluids).
- Multiple pregnancy twins.
- HDOP- high blood pressure disorder of pregnancy.
- Multi gravida.
- Prolonged labor.
- Infection.
- Obesity.
- Forceps and vacuum-assisted delivery.
Symptoms of PPH
- Uncontrolled bleeding.
- Decrease blood pressure.
- Increase pulse rate.
- Decrease red blood cell count.
- Dizziness and fainted.
Diagnosis
- Severe vaginal bleeding.
- Blood investigation – CBC
- Check for vitals.
Management of postpartum hemorrhage
Here are some important points. that how to do active management of PPH in its early stages.
- The doctor should find out the cause of PPH. and stop the cause of bleeding first.
- Uterine massage- which stimulates uterine contractions.
- Medicines- which help in uterine contractions- like oxytocin.
- Exploration of the uterine cavity for removing placental tissue.
- Repair vaginal tear and cervical tear.
- Bakri balloon and Foley catheter insert Intrauterine. Bakri balloon or Foley catheter to pressure on the bleeding in the uterus. if the Bakri balloon is not available then the uterus is packed with sterile gauze, sponge, and roller gauze.
- Leprotomy- open abdominal surgery to find out the cause of PPH and feel the bleeding vessels by repairing structure sites.
- Hysterectomy:- If the above management does not help to stop this thing lastly they should remove the uterus.
- Blood transfusion in case of excessive blood loss. A blood transfusion may be required to prevent shock and IV Fluids are also required to prevent sock.
Complication of PPH
Complications of postpartum hemorrhage (PPH) can be severe and potentially life-threatening if not promptly managed. These complications include:
- Shock: Excessive blood loss can lead to hypovolemic shock, where the body’s organs and tissues do not receive enough oxygen and nutrients due to insufficient blood volume.
- Organ Failure: In severe cases of PPH and shock, organs such as the kidneys, liver, and lungs may fail due to inadequate blood flow and oxygenation.
- Disseminated Intravascular Coagulation (DIC): Prolonged or severe bleeding can trigger DIC, a condition where blood clotting factors are consumed excessively, leading to both excessive bleeding and abnormal clotting throughout the body.
- Infection: Procedures and interventions performed to manage PPH, such as uterine exploration or surgical interventions, can increase the risk of infection, including endometritis (infection of the uterus).
- Anemia: Significant blood loss can lead to acute anemia, resulting in fatigue, weakness, and potentially requiring blood transfusions to restore normal red blood cell levels.
- Maternal Mortality: In extreme cases where PPH is not effectively controlled, maternal death can occur due to the combination of severe blood loss and associated complications.
- Psychological Impact: Experiencing severe complications during childbirth, including PPH, can have long-lasting psychological effects on the mother, affecting her emotional well-being and bonding with the newborn.
Management of PPH focuses on rapid assessment, identification of the underlying cause, and immediate intervention to control bleeding and stabilize the patient. Timely administration of medications, surgical interventions if necessary, and supportive care are crucial to minimizing these potential complications and ensuring maternal recovery.
References:
- American College of Obstetricians and Gynecologists. (2020). Practice Bulletin No. 183: Postpartum Hemorrhage. Obstetrics & Gynecology, 136(4), e49-e69. doi:10.1097/AOG.0000000000004188
- World Health Organization. (2012). WHO recommendations for the prevention and treatment of postpartum hemorrhage. Geneva: World Health Organization.
- Callaghan, W. M., Kuklina, E. V., & Berg, C. J. (2010). Trends in postpartum hemorrhage: United States, 1994-2006. American Journal of Obstetrics and Gynecology, 202(4), 353.e1-353.e6. doi:10.1016/j.ajog.2009.10.899
Also, Read
Ectopic pregnancy symptoms cause management
What is the Placenta, Types, and Functions
Abruptio Placentae Types signs & Management
Placenta Previa: Its Types and Management